Does immersive virtual reality (IVR) serve as a viable option for inclusion in medical training curricula? This was a question that McMaster University’s study set out to explore. The study, funded by Social Sciences and Humanities Research Council (SSHRC), was conducted by the university’s Department of Pediatrics as part of the McMaster Education Research Innovation and Theory (MERIT) program in partnership with a leading creator of XR medical simulations, MedVR Education. The objective was to gain faculty and trainee perceptions regarding the benefits, challenges and “potential incorporation of IVR” in medical training.
Entrustable Professional Activities (EPA) in medical education
Virtual reality is gaining inroads into many fields as a means of training and development. The healthcare sector is not an exception. Though being adopted by many organizations and institutes for training and practice purposes, the question still looms about its viability. Is it possible to be real-world ready by practicing in virtual environments with virtual patients? In the medical training landscape, Entrustable Professional Activities (EPAs) are considered to be a key factor in assessing competencies of trainees. EPAs refer to discrete units of professional tasks that practitioners are expected to perform independently during their training. According to the Association of American Medical Colleges (AAMC), EPAs offer a “framework for the guidelines because they offer a practical approach to assessing competence in real-world settings.” These EPAs serve as benchmarks to help track the competence of medical students and residents.
Though EPAs are of significant value during the training duration, they have challenges associated with them. Trainees often fail to meet the minimum EPA requirement due to factors like time constraints, unavailability of cases, or due to certain logistic issues. These limitations can result in producing healthcare professionals under-prepared to face real-world challenges, which in turn can risk patient outcomes.
Bridging the skill gap with VR training
Virtual reality training offers learners the opportunity to train in virtual environments mimicking real-world scenarios. Learners interact with virtual patients and virtual objects to perform procedures. With VR there is no requirement for an elaborate physical set-up, time is not a constraint, and training can be taken at any given hour during a day. All that a learner needs are a headset and a room to practice a scenario, any scenario. As Dr. Elif Bilgic, PhD, Assistant Professor & Education Scientist, McMaster University, says, “Based on the results of our study, faculty and fellows found that IVR is helpful in allowing learners to complete a scenario multiple times without needing additional equipment, especially helpful for scenarios that require an algorithmic approach and focus on non-technical skills.”
Realizing the benefits of VR training and understanding the risks associated with insufficient EPAs, the possibility of including virtual reality training as a means to gain experience and exposure to cases was considered by McMaster University’s (MERIT) program. This study included both faculty and residents as participants. They tried out pediatric cases like Pediatric Anaphylaxis as part of the study.
The objective of the study was to test the viability of virtual reality training in medical training curricula as a tool to achieve required EPA exposures.

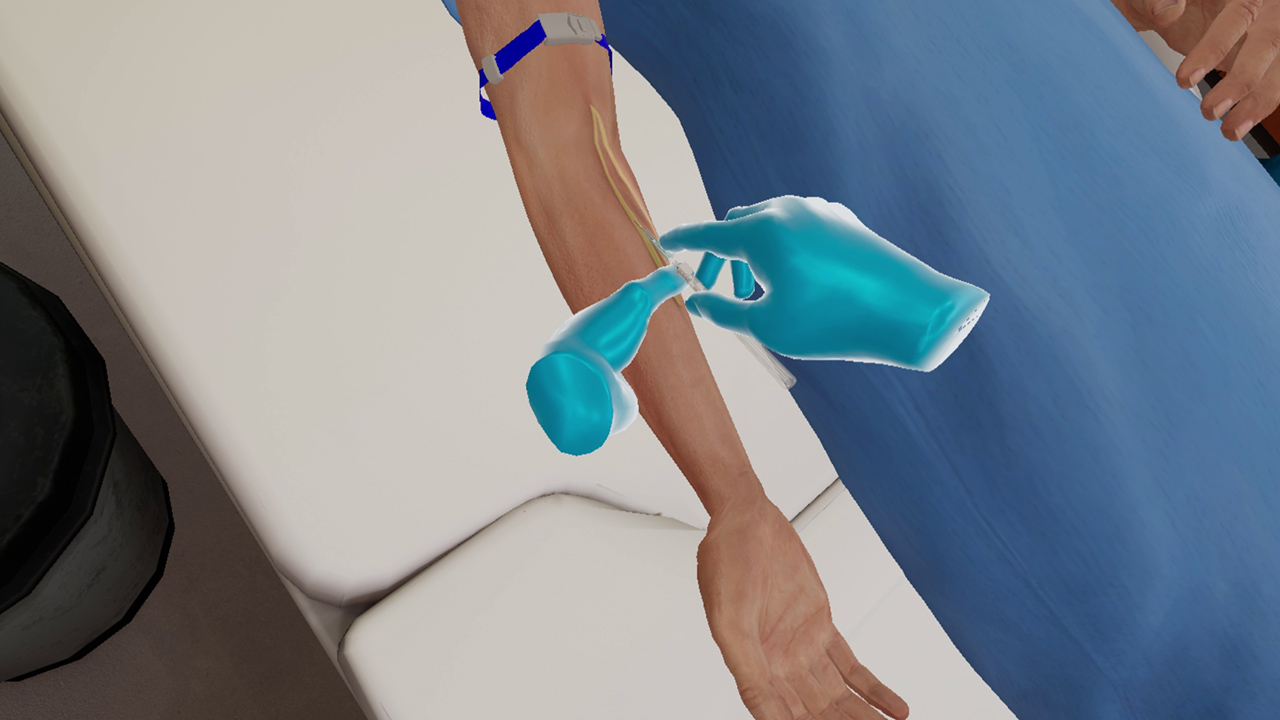
Managing a case of pediatric anaphylaxis in VR
Participants and methodology
As part of this study, both faculty and residents came together to explore medical scenarios through the medium of virtual reality. During these training sessions, participants were placed in scenarios that tested their clinical judgment skills, patient communication, decision-making, and their skills at performing procedures. These virtual scenarios were created to replicate real-world situations offering participants a high degree of realistic immersive training experience.
Having experienced their virtual scenarios, participants were invited to share their experience and feedback through in-depth interviews. Participants were recruited until thematic sufficiency was achieved and halted once it was certain that no new data was emerging. This method of collecting data ensured a broad and detailed understanding of experiences and views on the methodology were included in the study.
The reflexive thematic analysis method was used to transcribe and analyze the interviews. This method focuses on identifying themes and patterns within qualitative data and is a method suitable for a complex issue like the one at hand. It provides scope to deeply examine the perceptions and feedback of participants.
VR as a viable option for healthcare training
An analysis of participant feedback revealed that VR was accepted as a viable option for medical training purposes. One of the significant factors proved to be the realism it provided. Participants found themselves in realistic scenarios that closely replicated the conditions in which they would be required to perform. This included the AI-powered interaction with patients and family members, the resemblance to urgencies in scenarios and the changing conditions of patients. “Participants valued the heightened sense of realism with the patient’s clinical presentation, the patient’s room, and conversation with the family member, given their AI responses tailored to each question,” said Dr Elif Bilgic. Practicing in these conditions was favorable in helping them prepare for real-world challenges.
An important piece of feedback came regarding the selection of the content difficulty level. Participants were of the opinion that the complexity of VR scenarios should be based on the competency and level of expertise of the participants. They also pointed out that customization of simulations should be tailored to add maximum value to the training. It should be appropriately challenging to participants.
Conclusion
A unanimously positive feedback indicated towards participants accepting that VR has “potential in EPA training and assessment.” At the same time, they believed that the objectives of this training should consider the trainees’ competency level.
This might be a small study conducted by a university towards the inclusion of VR training in medical training curricula, but it has shown some very promising results. It helps learners prepare for real-world challenges, provides ample practice opportunities in a variety of cases, exposing them to rare but possible instances they may come across in real life. In the words of Dr. Elif Bilgic “Overall, we believe that our partnership was very fruitful and allowed us to understand in-depth the potential role of IVR in medical education, providing us with new directions regarding scholarship and educational initiatives.”
About MedVR Education:
MedVR Education is a continuing education platform, founded with the specific aim of providing immersive and engaging VR training solutions to healthcare professionals. Its dynamically growing library witnesses the addition of 4-5 new solutions every month. MedVR Education is at the forefront of implementing the latest technology in the field of VR and training, ensuring that learners get the best possible learning experience.
Contact us to know more about VR in healthcare training or visit MedVR Education to explore the various programs we offer.